The Impact of Meniere’s Disease on Hearing and Balance
Meniere’s Disease is a rare, chronic inner ear disorder that disrupts hearing and balance. This condition causes episodes of vertigo, tinnitus, and progressive hearing loss, which can vary in intensity. The exact cause of Meniere’s Disease remains unknown, but it likely results from a combination of genetic and environmental factors.
How Meniere’s Disease Disrupts the Inner Ear
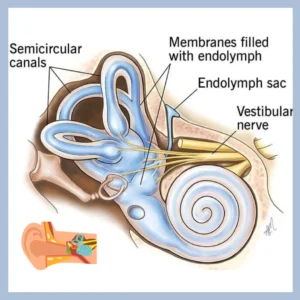
The inner ear plays a vital role in both hearing and maintaining balance. It contains two critical structures: the cochlea, responsible for processing sound, and the vestibular system, which helps regulate balance. Meniere’s Disease disrupts the normal function of these structures by causing an abnormal buildup of fluid known as endolymph within the inner ear. This excess fluid leads to a range of issues that can significantly impact your daily life.
The Cochlea and Hearing Disruption
The cochlea is a spiral-shaped organ filled with fluid and lined with tiny hair cells that respond to sound waves. These hair cells translate sound vibrations into electrical signals, which the auditory nerve sends to the brain. When Meniere’s Disease causes endolymph to accumulate in the cochlea, it disrupts this delicate process. The increased fluid pressure can damage or destroy the hair cells, leading to hearing loss. This hearing loss can fluctuate, sometimes returning to normal between episodes, but it often deteriorates over time, becoming permanent.
The Vestibular System and Balance Issues
The vestibular system, located adjacent to the cochlea, is crucial for maintaining balance and spatial orientation. It includes the semicircular canals and otolith organs, which detect head movements and changes in position relative to gravity. In Meniere’s Disease, the excess fluid in the vestibular system interferes with its normal function, sending inaccurate signals to the brain about the body’s position and movement. This miscommunication results in vertigo—a spinning or tilting sensation—even when standing still. The vertigo can be intense and unpredictable, leading to dizziness, unsteadiness, and an increased risk of falls.
The Broader Impact on Hearing and Balance
The fluid imbalance caused by Meniere’s Disease affects hearing and balance and their interaction. For example, during a vertigo episode, you might also experience a sudden drop in hearing clarity, particularly in one ear. Tinnitus, or ringing in the ear, often accompanies these episodes, further complicating your ability to hear and maintain balance. These symptoms can make everyday tasks like walking, driving, or even having a conversation challenging.
Understanding how Meniere’s Disease disrupts the inner ear highlights the condition’s complexity and the importance of seeking professional help. By managing fluid buildup and protecting the inner ear’s delicate structures, treatments can help reduce the frequency and severity of symptoms, preserving hearing and balance as much as possible.
The Progressive Nature of Hearing Loss in Meniere’s Disease
Hearing loss in Meniere’s Disease is often gradual, with its severity increasing over time. This progressive nature is a vital characteristic of the condition, making it particularly challenging for those affected. Understanding how and why this hearing loss develops can help individuals better manage the disease and seek appropriate treatment early.
Fluctuating Hearing Loss: An Early Sign
In the initial stages of Meniere’s Disease, hearing loss may not be constant. Instead, it often fluctuates, meaning that a person’s hearing can vary from day to day or even within the same day. During a Meniere’s episode, hearing may suddenly worsen, particularly for lower frequencies, only to improve partially or almost entirely afterward. This unpredictable pattern can be confusing and frustrating, as it may give the false impression that hearing is returning to normal when the disease progressively worsens.
The Transition to Permanent Hearing Loss
As Meniere’s Disease progresses, the episodes of hearing loss typically become more frequent and severe. The once-temporary declines in hearing can gradually become a constant state of reduced hearing. This transition from fluctuating to permanent hearing loss marks a significant progression in the disease. In some cases, this permanent hearing loss may only affect one ear, while in others, it could eventually involve both ears.
Sensorineural Hearing Loss: The Long-Term Effect
Over the long term, Meniere’s Disease can lead to sensorineural hearing loss, which results from damage to the inner ear structures or the auditory nerve. Unlike conductive hearing loss, which can often be treated or managed with medical intervention, sensorineural hearing loss is typically irreversible. This type of hearing loss is difficulty hearing faint sounds and understanding speech, particularly in noisy environments.
Living with Progressive Hearing Loss
Living with progressive hearing loss due to Meniere’s Disease can be challenging. It not only affects a person’s ability to hear but also impacts their communication, social interactions, and overall quality of life. People may find it increasingly difficult to engage in conversations, enjoy music, or hear warning signals, leading to isolation and frustration. As hearing loss becomes more pronounced, the need for assistive devices like hearing aids may become essential.
The progressive nature of hearing loss in Meniere’s Disease underscores the importance of early diagnosis and proactive management.
Risk Factors and Potential Causes of Meniere’s Disease
While the exact cause of Meniere’s Disease remains unclear, several factors may increase the risk. These include:
- Age: Meniere’s Disease most commonly affects people between 40 and 60.
- Sex: Some studies suggest that women may be slightly more prone to this condition.
- Genetics: A family history of Meniere’s Disease could increase your risk.
- Autoimmune Diseases: Conditions like rheumatoid arthritis and lupus may elevate the risk.
Researchers continue studying these factors to understand their connection to Meniere’s Disease better.
Managing Meniere’s Disease: Treatment and Lifestyle Adjustments
Though chronic and often debilitating, you can manage Meniere’s disease effectively through a combination of medical treatments and lifestyle changes. While there is no cure, these strategies can significantly reduce the frequency and severity of symptoms, helping individuals lead a more comfortable and balanced life.
Medical Treatments for Meniere’s Disease
Managing Meniere’s Disease often begins with medical treatment aimed at controlling symptoms and preventing further progression of the condition. These treatments address the specific symptoms each individual experiences, such as vertigo, hearing loss, and tinnitus. Several types of medications are commonly prescribed to manage Meniere’s Disease symptoms:
- Diuretics (Water Pills): Diuretics help reduce fluid retention in the body, including the inner ear, which can alleviate pressure and reduce the severity of vertigo attacks.
- Betahistine: This medication improves blood flow to the inner ear, helps reduce fluid pressure, and controls symptoms like vertigo.
- Anti-nausea and Motion Sickness Medications: These medications, such as meclizine or diazepam, manage the nausea and dizziness accompanying vertigo episodes.
- Steroid Injections: In some cases, steroids are injected directly into the middle ear to reduce inflammation and control vertigo.
Therapies and Devices
- Vestibular Rehabilitation Therapy (VRT): VRT is a specialized form of physical therapy focusing on improving balance and reducing dizziness. It involves exercises designed to help the brain adapt to the changes in balance signals caused by Meniere’s Disease.
- Hearing Aids: Hearing aids can be valuable for those experiencing hearing loss. They amplify sound and improve speech understanding, making communication easier in daily life.
- Surgical Options: In severe cases of Meniere’s Disease where other treatments have failed, doctors may consider surgery:
- Endolymphatic Sac Procedure: This surgery relieves pressure by draining excess fluid from the inner ear. A small tube (stent) may be placed to facilitate ongoing fluid drainage.
- Vestibular Nerve Section: This procedure involves cutting the vestibular nerve to prevent vertigo attacks while preserving hearing.
- Labyrinthectomy: This surgery removes the balance organs in the inner ear, effectively eliminating vertigo but also causing total hearing loss in the affected ear. It is typically considered only when the hearing loss is already profound.
Lifestyle Adjustments to Manage Meniere’s Disease
In addition to medical treatments, certain lifestyle adjustments can significantly help manage Meniere’s Disease. These changes can help reduce the triggers of symptoms and improve overall well-being.

Dietary Changes:
- Low-Sodium Diet: Reducing sodium intake is crucial for managing Meniere’s Disease. Excess salt can lead to fluid retention, worsening the pressure in the inner ear. You should limit sodium to no more than 1,500 milligrams per day.
- Avoiding Caffeine and Alcohol: Both caffeine and alcohol can exacerbate symptoms by affecting fluid balance and blood flow in the inner ear. Limiting or avoiding these substances may help reduce the frequency of attacks.
- Monitoring Fluid Intake: While staying hydrated is important, it’s also essential to monitor fluid intake to prevent excess fluid buildup in the body.
Stress Management:
- Stress Reduction Techniques: Stress is known to trigger or worsen Meniere’s Disease symptoms, particularly vertigo. Incorporating stress reduction techniques like deep breathing exercises, meditation, and mindfulness can help manage stress levels.
- Regular Exercise: Regular, moderate exercise can improve overall health, reduce stress, and enhance balance, which may help mitigate symptoms.
- Adequate Rest: Ensuring sufficient sleep and rest is essential, as fatigue can contribute to the severity of symptoms.
Environmental and Lifestyle Modifications:
- Noise Management: In environments with high noise levels, individuals with Meniere’s Disease should consider using ear protection to reduce the impact on their hearing.
- Safe Environment: Creating a safe living environment is crucial to prevent falls, particularly during vertigo episodes. This may include installing grab bars in the bathroom, using non-slip mats, and keeping walkways clear of obstacles.
- Regular Monitoring: Journaling about symptoms and potential triggers can help identify patterns and allow for better management of the condition.
Combining Treatment and Lifestyle for Effective Management
Managing Meniere’s Disease effectively requires a comprehensive approach combining medical treatments and lifestyle adjustments. By addressing the condition’s physical and emotional aspects, people can significantly reduce the impact of symptoms on their daily lives. Regular consultations with healthcare providers, particularly audiologists and specialists in vestibular disorders, are essential to adapting treatment plans as needed and ensuring the best possible quality of life.
Take the Next Step Toward Better Hearing and Balance
Don’t let Meniere’s Disease control your life. Contact Stanford Hearing today to schedule a consultation and explore treatment options tailored to your needs. Your path to better hearing and balance starts here.
